Several weeks ago, the death of Jamie Garcia—a worker at a state-licensed cannabis cultivation site in Los Angeles—during an ICE raid sent shockwaves through the medical cannabis community. With more than six million patients relying on these programs nationwide, and the majority of U.S. states having legalized medical cannabis in some form, Garcia’s death is more than a tragedy. It’s a warning.
This comes on the heels of another blow: President Trump’s FY2026 budget proposal eliminates a longstanding provision in the Commerce, Justice, Science, and Related Agencies (CJS) Appropriations bill that prevents the Department of Justice (DOJ) and Drug Enforcement Administration (DEA) from interfering with state-authorized medical cannabis programs.
Since 2014, this provision—known as the CJS Medical Cannabis Amendment—has functioned as a fragile but critical ceasefire between federal authorities and state-level programs. It has protected patients, providers, caregivers, and state employees from arrest, prosecution, and asset forfeiture. Before its passage, the DOJ executed more than 500 paramilitary-style raids on medical cannabis facilities, threatened state employees, and aggressively prosecuted patients and providers. This amendment was never intended to be permanent, but until comprehensive legislation is passed, it remains the only federal protection patients have.
Now, with the amendment in jeopardy and recent Medicaid cuts passed in Trump’s “Big Beautiful Bill,” the medical cannabis community is on high alert. The loss of both healthcare coverage and access to cannabis-based medicine would be devastating—especially for low-income patients, seniors, veterans, and people living with chronic or terminal illnesses.
For millions of Americans living with epilepsy, cancer, PTSD, multiple sclerosis, rare diseases, and chronic pain, cannabis is not an “alternative lifestyle choice.” It is the only effective treatment—or the only one without debilitating side effects. In fact, studies have shown that states with medical cannabis laws experience a 23% reduction in opioid overdose deaths and a nearly 20% drop in opioid prescriptions by orthopedic surgeons.
The federal government’s own agencies have begun to catch up. In 2024, the Department of Health and Human Services (HHS) formally recommended moving cannabis to Schedule III, acknowledging for the first time that it has accepted medical use. Yet rather than opening the door to progress, this shift was quickly buried under misinformation and political distraction.
Ahead of the FY2026 CJS Appropriations bill markup, more than 40 national organizations—including the Epilepsy Foundation, National MS Society, U.S. Pain Foundation, AIDS Action, and Iraq and Afghanistan Veterans of America— signed on to a letter urging Congress to preserve the CJS Amendment. 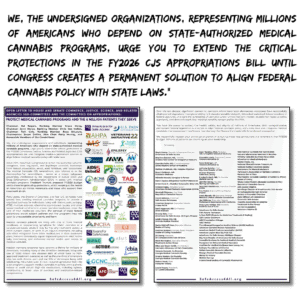
“We, the undersigned organizations, representing millions of Americans who depend on state-authorized medical cannabis programs, urge you to extend the critical protections in the FY2026 CJS Appropriations bill until Congress creates a permanent solution to align federal cannabis policy with state laws.”
On July 15th, the CJS Appropriations Committee went against President Trump’s proposal to omit protections for state medical cannabis laws but added a claw-back provision and moved to block the rescheduling process currently underway at the DEA from advancing. In a vote split along party lines, the CJS appropriations bill advances to the full Appropriations Committee at a date yet to be determined. It will also need to pass through the Senate appropriations process.
This addition could be a poison pill for access for many patients. While most state legal medical cannabis businesses conform to state-sensitive use rules (i.e., 600 feet from a school), the provisions in the inserted language would allow raids on any facilities that don’t conform to parameters listed in 21 U.S.C. 860 but would also enable DOJ to apply double penalties to business in the crosshairs of state and federal laws.
These state medical cannabis programs are not experimental or fringe. Forty states, the District of Columbia, and four U.S. territories have enacted comprehensive systems, and another nine offer limited medical access. Patients report improved sleep, function, and quality of life. Many reduce or eliminate opioids, benzodiazepines, and other high-risk medications.
Older Americans are leading this shift. Cannabis use among seniors has doubled, with most treating arthritis, chronic pain, insomnia, and anxiety. This shift supports the emerging medical field of deprescribing—a public health necessity as 750 seniors are hospitalized daily due to preventable adverse drug reactions.
The science is clear. The National Academies of Sciences found conclusive evidence supporting cannabis in treating chronic pain, chemotherapy-induced nausea, and MS-related spasticity. Meanwhile, opioid misuse costs the U.S. $35 billion annually. Chronic pain alone affects one in three adults, doubles suicide risk, and drains over half a trillion dollars from our economy each year.
Cutting off access to medical cannabis makes no fiscal or ethical sense.
And for veterans, the consequences could be lethal—one in three lives with chronic pain. More than 22% already use cannabis-based treatments. Every day, 17.5 veterans die by suicide—many of whom have reported that cannabis helped them when other treatments failed.
The CJS Medical Cannabis Amendment is not a permanent fix—but it is a necessary one. It gives patients and providers breathing room while Congress moves toward a real solution. But ceasefires don’t become peace without action.
Now, with the medical value of cannabis formally recognized by HHS and FDA, the question before Congress is clear: Will they continue to protect state medical cannabis programs and find a permanent federal solution, or will they keep forcing patients to fight for their medicine year after year?
Take action today to protect patients. Click here
Learn more about Steph Sherer and her work through our featured piece on her in our Women in Cannabis section.